Shai M. Rozen, M.D., F.A.C.S.
1801 Inwood Road
Dallas, TX 75390
Phone: (214) 645-2353
Monday–Friday: 8 a.m.–5 p.m.
Eyelid Asymmetry
One of the most important areas to protect—and always a priority in facial asymmetry treatment—is the eye on the paralyzed side. Patients may have difficulties closing the eye or find it impossible to do so at all due to paralysis of the orbicularis oculi muscle that surrounds the eye. This condition is called paralytic lagophthalmos.
Dr. Shai Rozen, a leading specialist in the area of facial paralysis, and his team at the University of Texas Southwestern Medical Center offer passive and dynamic treatments for the eyelids to improve facial balance and protect the health of the eye. Early treatment is key to the quality of results and the health and functioning of the eye.
What happens when the eye can’t close properly?
Paralysis of the eyelid can expose the cornea, causing significant irritation characterized by redness, sensitivity, and a foreign body sensation. These symptoms are often worse in the morning after awakening because the eye remains open during the night. This condition is known as exposure keratopathy.
If left untreated, this condition may develop into ulcerations, scarring, and even blindness. Since the facial nerve innervates the lacrimal gland, which produces tears, facial paralysis patients not only have difficulty closing the eye, they experience dry eye due to decreased tearing.


Maintaining Lubrication of the Eye
The first step in the treatment of paralytic lagophthalmos, regardless of any planned surgeries, is to keep the eye lubricated at all times using a combination of eye drops and ointment. Occasionally, patients need to wear a moisture chamber, which is eyewear that protects the eye—especially during sleep—by maintaining moisture around the eye.
In cases of Bell’s palsy or facial paralysis after surgery, when many patients are expected to improve on their own or the situation is expected to resolve itself, lubrication may be the only treatment needed. Surgical solutions are needed when there is incomplete resolution or no recovery is expected.
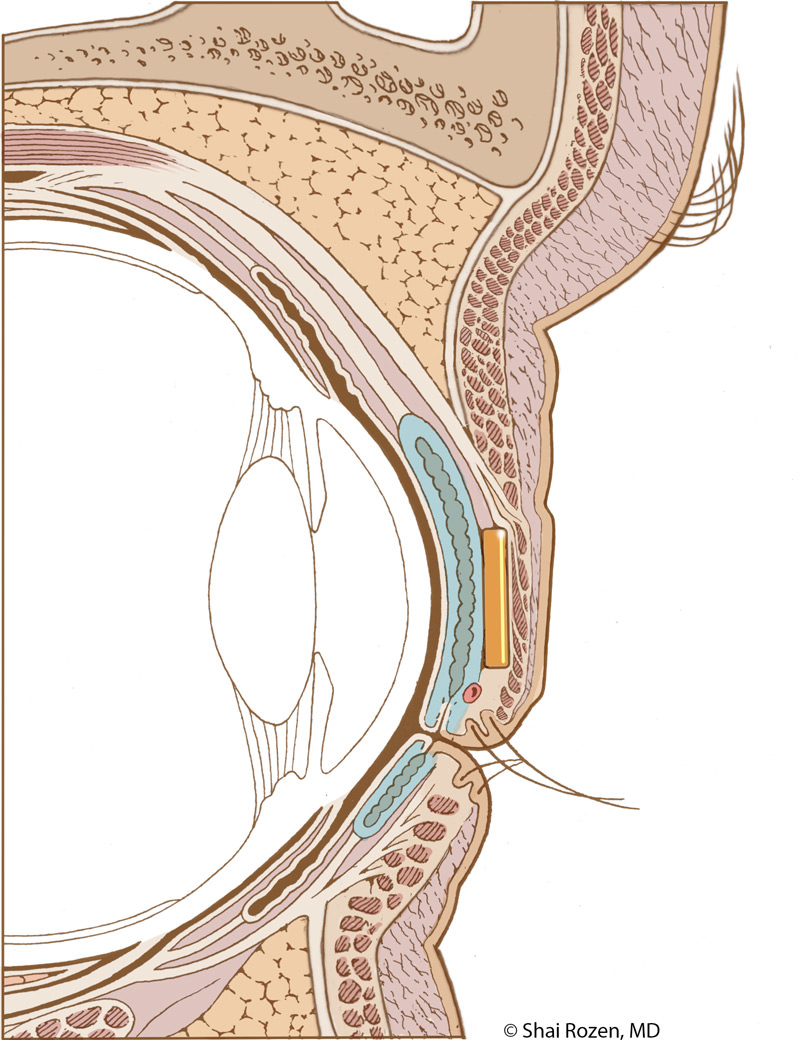
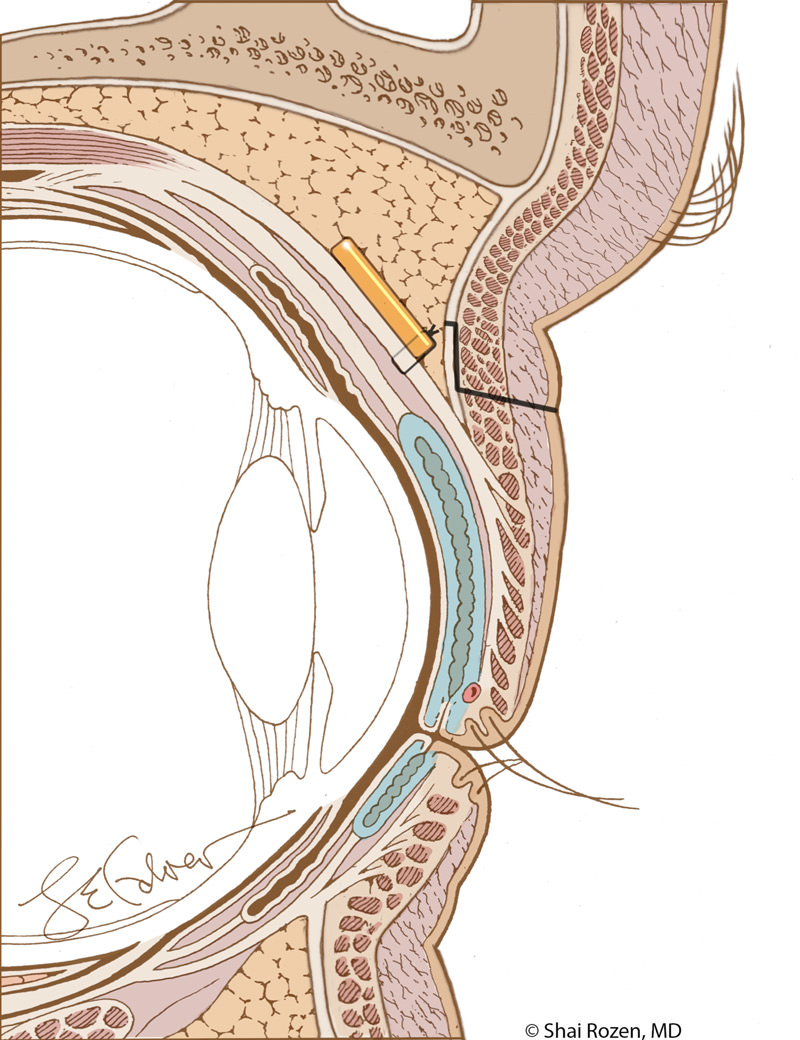
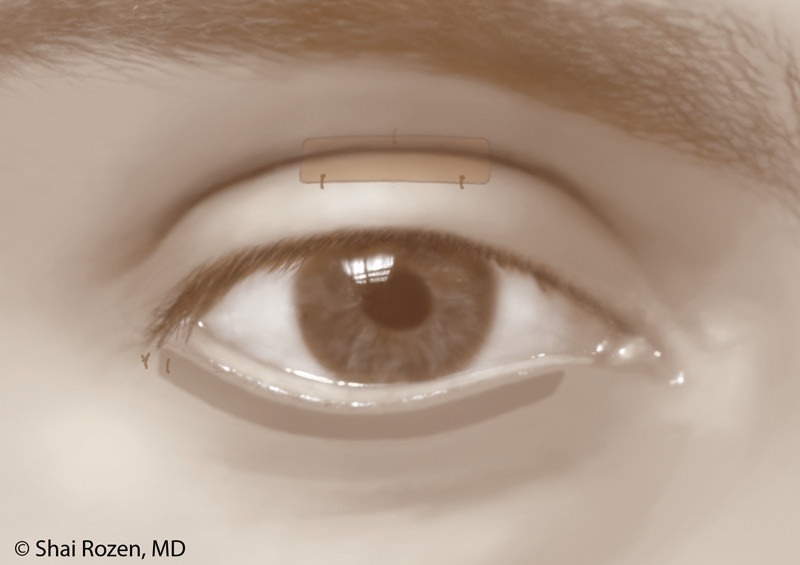
Upper Eyelid Weights
Among the more common surgical solutions to treat an inability to completely close the upper eyelid is the insertion of a weight made of gold or platinum in the upper eyelid. The principle behind this treatment is using gravity during sleep to protect the eye by closing the upper eyelid. These weights will often remain in the upper eyelid, but they may be removed or downsized if partial or complete recovery is observed.
Is the gold eyelid weight noticeable after surgery?
One of the main concerns patients have is whether a gold eyelid weight will be noticeable after surgery. Dr. Rozen’s goal for facial reanimation is to help the patient look as close as possible to the period prior to paralysis. This means details are extremely important. Traditional techniques fail to hide the weight well. They are too obvious and also, over time, risk extrusion. Dr. Rozen and his group felt that protection alone without aesthetic consideration is a suboptimal solution. For this reason, the group worked extensively in the anatomy lab in an attempt to modify current techniques, so the weight is better placed and hidden yet maintains its original purpose of protecting the eye.
In order to do so, we place a slightly heavier weight higher and deeper in the upper eyelid. Although mechanically, this is a less optimal position, the slightly heavier weight compensates, and the aesthetic result is considerably better. Extrusion is less likely with this technique and has not been encountered in more than several hundred of Dr. Rozen’s patients. 1
Dr. Shai Rozen
Dr. Rozen is a board-certified plastic surgeon who co-created a facial paralysis specialty group with colleagues from otolaryngology & neurosurgery at the University of Texas Southwestern Medical Center.
Meet Dr. Rozen
Surgery for Lower Eyelid Drooping
Patients often develop a situation in which a lower eyelid droops below the one on the uninjured side, exposing more of the white of the eye, called lower lid malposition. The lower eyelid can also turn inside out, a finding called ectropion.
Several procedures may be performed based on the severity and laxity of the lower eyelid. Most involve repositioning the lower eyelid while providing further support.
Canthoplasty
In younger patients with paralytic ectropion, who don’t have horizontal excess or laxity in the lower eyelid, sometimes repositioning of the lower lateral canthal ligament— the part that connects the lower lid to the orbit—can help elevate the lid to a more functional position. This is not a common procedure since most patients have some degree of horizontal laxity and need a lateral tarsal strip.
Lateral Tarsal Strip
When a patient has lower lid malpositioning or ectropion in addition to looseness of the lower eyelid, usually a tarsal strip is performed. In this procedure, the lower lid is slightly shortened on its side farthest from the nose, so when it is reattached to the orbit, it is not only in a higher position but also under proper tension. This helps position the lower lid in the correct position and improves both tear routing and lower corneal protection.
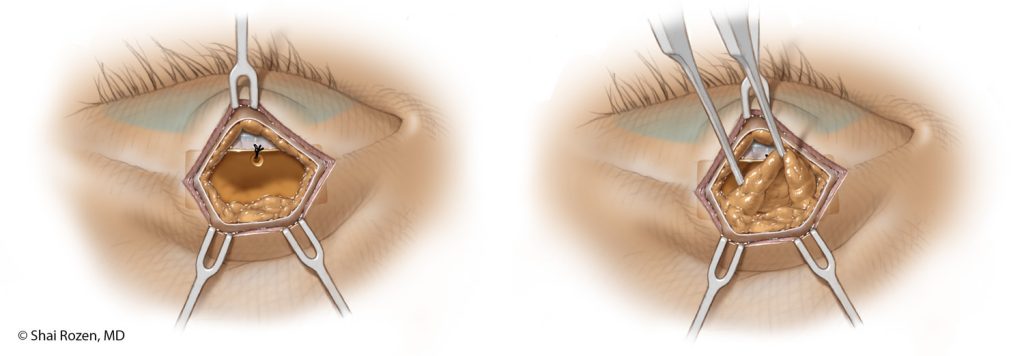
Fascial/Tendon Support of the Lower Eyelid
The lateral tarsal strip is a very effective procedure in lifting the lower eyelid into an improved position but has some minor drawbacks in some patients. These mainly are slight excess pulling sideways and also insufficient elevation of the medial lower eyelid (the side closer to the nose). In some patients, it leaves a small amount of excess corneal exposure of the lower inner cornea. For this reason, we will often insert a small graft extending from both sides of the orbital rim in order to lift the eyelid upwards equally from both sides. This provides a very good functional and aesthetic result without changing the original shape of the eye.
Can upper and lower eyelid procedures be performed together?
Although the lower eyelid moves less than the upper eyelid and takes a lesser role in corneal protection, its correct positioning is still critical to corneal integrity and proper management of tears. For that reason, we usually perform surgery of the lower and upper eyelids at the same time. If patients request, Dr. Rozen also performs upper and lower eyelid surgery on the healthy side to further improve facial balance.
Dynamic Strategies for Treating the Paralyzed Eye
Dynamic restoration means returning motion to the paralyzed side. Dynamic restoration of the eye area restores the ability to close the eye voluntarily and possibly some degree of the blink reflex.
Not all patients are candidates for this type of reconstruction, and several crucial factors are considered, of which the most important is the duration of paralysis. Patients with less than a year of paralysis, sometimes a bit longer, may still be candidates.
Dr. Rozen’s group has recently published one of the largest series of patients who underwent this type of approach and demonstrated improved corneal protection as well as improved closure dynamics of the eye, both in the degree of closure and speed of closure.2
Reconstruction procedures may include a combination of nerve transfers and nerve grafts in addition to the passive techniques described above. In appropriate candidates, the results are functionally and aesthetically superior to traditional techniques but also depend on how long a patient has had paralysis and whether the muscles of the face are salvageable.
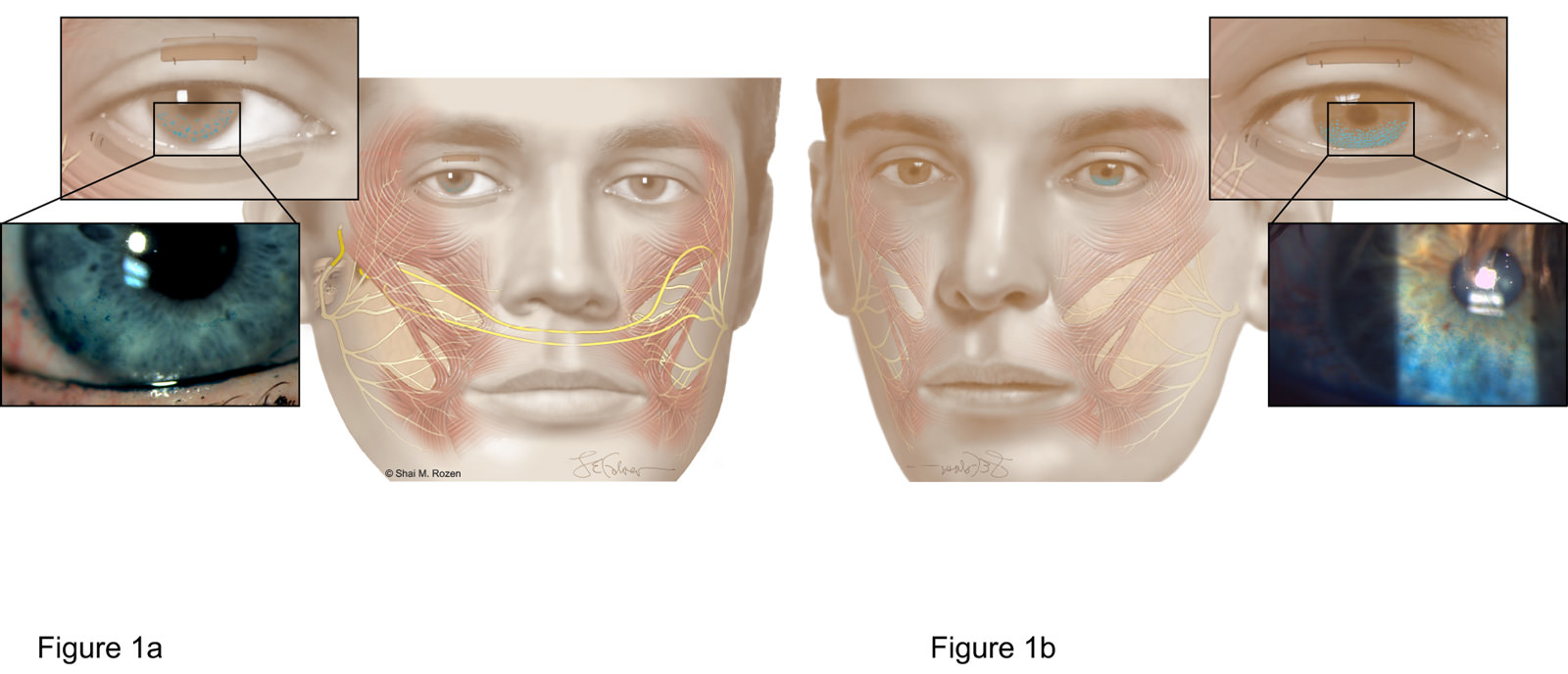
Dr. Rozen and his team compared the corneal integrity and ability to close the eyelids between 2 treatment groups. Figure 1a depicts patients who underwent dynamic reanimation of the eyelids with renervation techniques. Figure 1b depicts patients who could only undergo passive techniques for eye protection. Patients who underwent dynamic reanimation with renervation techniques (Figure 1a) had more corneal protection and improved eye closure in long-term follow-ups.
A Valuable Resource for Those Affected by Facial Paralysis
If you, a loved one, or a patient is affected by facial paralysis, it’s crucial to have accurate, up-to-date information about symptoms and solutions. Board-certified plastic surgeon Dr. Shai Rozen, a specialist in facial paralysis and facial aesthetics, created Your Guide to Facial Paralysis & Bell’s Palsy to be a readily accessible resource for all.
This downloadable, printable e-book makes it easy to understand:
- How paralysis affects the face
- When it’s time to see a specialist
- Common causes of facial paralysis
- The difference between facial paralysis and Bell’s palsy
- Myths and facts
- The latest treatment options
- Answers to common questions
Get your free copy today—to download or view in your web browser—by completing the following fields:

Next Steps
For more information about improving eyelid symmetry related to facial palsy, request a consultation to meet with Dr. Rozen at UT Southwestern.
1Upper eyelid post-septal weight placement for treatment of paralytic lagophthalmos. Plast Reconstr Surg. 2013 Jun; 131(6):1253-65. DOI: 10.1097/PRS.0b013e31828be961. PMID: 23714789.
2 Orbicularis Oculi Muscle Reinnervation Confers Corneal Protective Advantages over Static Interventions Alone in the Subacute Facial Palsy Patient. Plast Reconstr Surg. 2020 Mar;145(3):791-801. DOI: 10.1097/PRS.0000000000006608. PMID: 32097327 (March 2020 Cover Article)