Shai M. Rozen, M.D., F.A.C.S.
1801 Inwood Road
Dallas, TX 75390
Phone: (214) 645-2353
Monday–Friday: 8 a.m.–5 p.m.
Nerve Transfer
Facial paralysis, in most cases, is caused by damage to the facial nerve and results in the inability to move the facial muscles. If performed early enough before irreversible damage to the facial muscles occurs, nerve transfers in combination with other procedures can effectively restore function, appearance, and facial balance.
Dr. Shai Rozen, a facial paralysis specialist who is known nationally and internationally for his innovative work in the field of facial paralysis, and a group of leading neurosurgeons and neurotologists at the University of Texas Southwestern Medical Center, have a broad experience and expertise in the latest techniques for restoring facial function in patients with facial paralysis. The following page explains to patients how nerve transfers are used to restore facial function, appearance, and harmony, as well as self-confidence for patients from across the U.S. and around the globe.
What is a nerve transfer?
A nerve transfer in the setting of facial paralysis involves disconnecting a non-facial nerve, then transferring and connecting it to the injured facial nerve. The purpose of a nerve transfer is to allow nerve fibers (axons) from the donor nerve (in this case, the non-facial nerve which is cut) to grow into the facial nerve in order to reach the muscles of the face and subsequently activate them. This will, in essence, allow us to salvage the facial muscles and avoid irreversible atrophy (death) of these muscles. If the facial muscles are irreversibly damaged, it is necessary to transplant a functional muscle in their stead.
This figure depicts several different configurations of nerve transfers, in this scenario, nerve to masseter transfer to facial nerve, as described by Dr. Rozen on the subject. Zhang S, Hembd A, Ching CW, Tolley P, Rozen SM. Early Masseter to Facial Nerve Transfer May Improve Smile Excursion in Facial Paralysis. Plast Reconstr Surg Global Open. 2018 Nov 15;6(11):e2023. DOI: 10.1097/GOX.0000000000002023. PMID: 30881808.
Who are candidates for nerve transfers?
Nerve transfers cannot be performed on everyone. The main determinant of whether someone is a candidate for a nerve transfer is the duration of the paralysis. If a person has had paralysis for longer than 18 months and has no evidence of facial muscle activity, the chances of salvaging these muscles via nerve transfers are low. For nerve transfers to work, the target muscles—the facial muscles, must be salvageable. After 18 months without innervation, the facial muscles atrophy and suffer irreversible damage, needing to be replaced by transplanting a functional muscle.
What are the advantages of nerve transfers for facial paralysis?
The advantage of nerve transfers is that they can help salvage a patient’s own facial muscles and activate the face in many ways similar to before the injury. With different combinations of nerve transfers and additional cross facial nerve grafts (CFNG) targeting different portions of the face, we can separately innervate different facial muscle subunits such as those responsible for the smile, some responsible for eye closure, and even mouth closure.
Dr. Shai Rozen
Dr. Rozen is a board-certified plastic surgeon who co-created a facial paralysis specialty group with colleagues from otolaryngology & neurosurgery at the University of Texas Southwestern Medical Center.
Meet Dr. Rozen
Which nerves are used as donor nerves for facial paralysis?
There are several options for donor nerves, but currently, the most commonly used is the masseteric nerve, also called the nerve to masseter (NTM). This nerve is a branch of the trigeminal nerve, also called the fifth cranial nerve, and its job in nature is to activate the masseter muscle, which is a strong masticatory (chewing) muscle.
It is important to understand that it is very rare that Dr. Rozen would need to use the entire nerve; nearly always just a branch of the nerve is needed, so the function of the masseter muscle is preserved. Even in the rare cases that the entire nerve is used (in complex cases when the nerve might be reused as previously published by Dr. Rozen), the function of mastication remains undisturbed. In rare cases, Dr. Rozen may use portions of the spinal accessory or hypoglossal nerves.
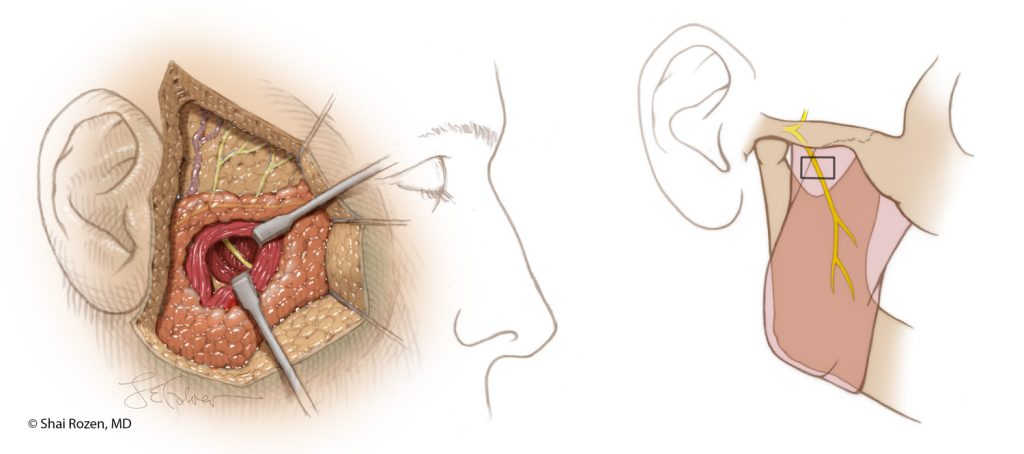
These figures depict the anatomy and position of the masseter nerve, which is often used in both nerve transfers and functional muscle transplants in facial reanimation as described in a publication by Dr. Rozen. A Reliable Anatomic Approach for Masseter Nerve Dissection in the Setting of Facial Reanimation. J Plast Reconstr Aesthet Surg. 2013 May; 66(10). DOI: 10.1016/j.bjps.2013.04.009.
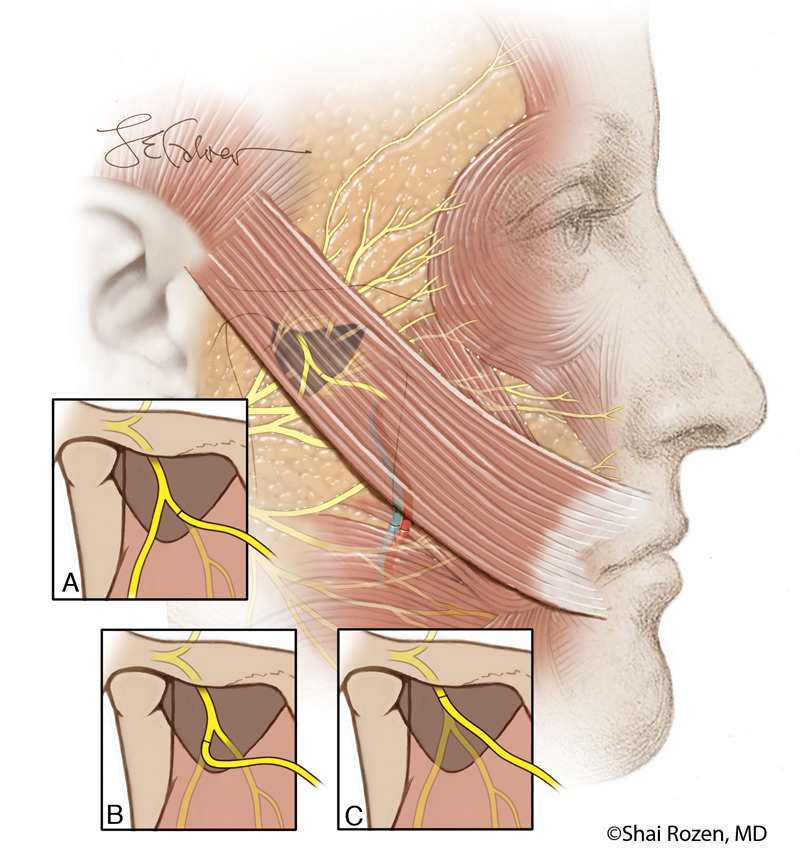
This figure depicts a side view of a transplanted muscle being innervated in one stage by a nerve to masseter. This is depicted in Dr. Rozen’s article on different salvage techniques with the nerve to masseter in difficult cases. The reuse of the nerve to masseter may be performed in both cases or nerve transfers if performed early enough or more commonly in cases of failed free functional muscle transplants. Reuse of The Masseteric Nerve for Dynamic Reanimation in Facial Palsy Patients with Previously Failed One-Stage Dynamic Smile Reanimation. Plast Reconstr Surg. 2019 Feb; 143(2):567-571; DOI: 10.1097/PRS.0000000000005253. PMID: 30688904.
During a nerve transfer, is the donor nerve attached to the entire facial nerve or just part of it?
How much of the paralyzed facial nerve is used for reanimation in cases of nerve transfers depends on the current function of the facial nerve as well as its potential for recovery. If the facial nerve is completely paralyzed and has no chance of recovery, we connect the donor nerve into the trunk of the facial nerve—a truncal transfer. If the facial nerve provides some tone or is only partially paralyzed, we use very specific branches of the facial nerve–a branch transfer.
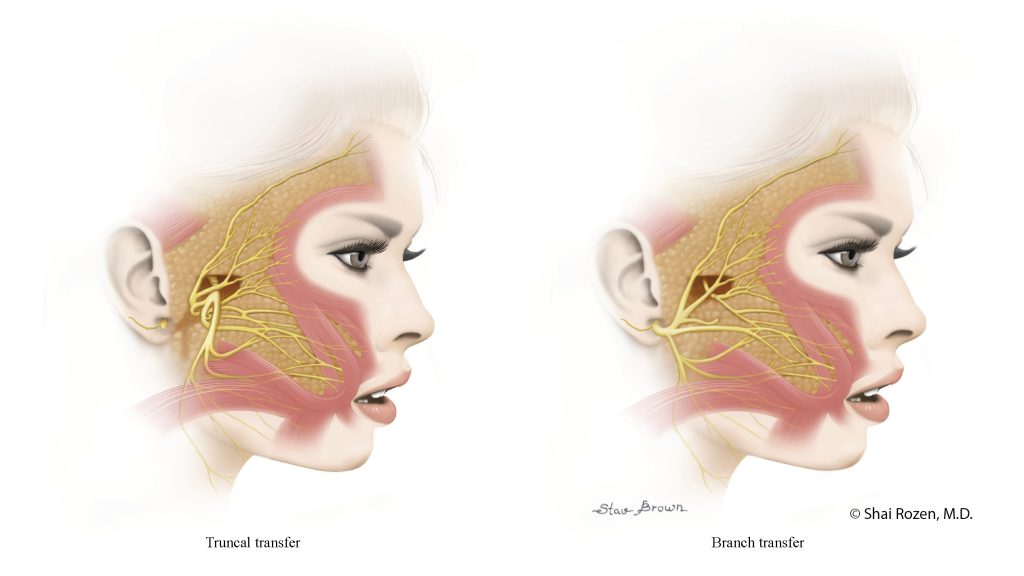
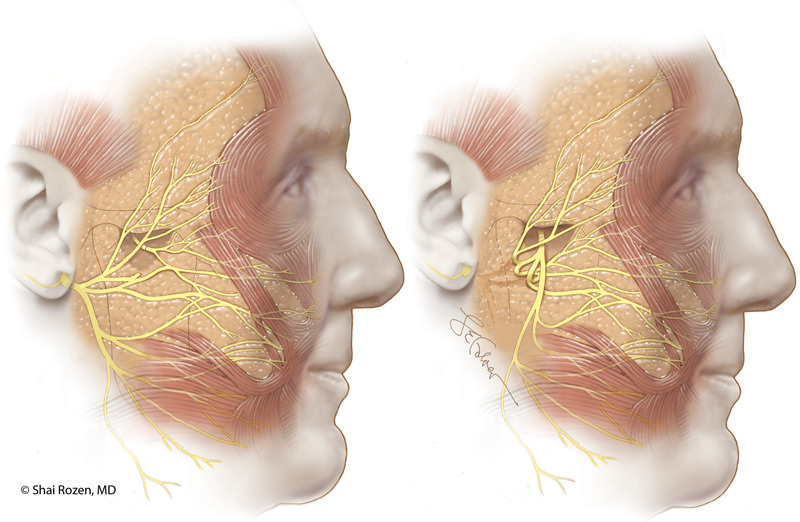
This figure depicts two types of nerve transfers that are used depending on the patient’s current condition and chances of future recovery. This is described by Dr. Rozen in the following article: Facial Nerve Trauma: Clinical Evaluation and Management Strategies. Plast Reconstr Surg. 2019 May; 143(5):1498-1512. DOI: 10.1097/PRS.0000000000005572. PMID: 30807496.
How can a nerve other than the facial nerve restore facial muscle function since nature didn’t design it to do so?
Indeed, there is no better nerve for reconstructing the facial nerve than the facial nerve itself. It provides tone, synchroneity (coordinated timing of smiling between both sides of the face), and spontaneity (a smile that occurs when an emotion evokes a smile and we don’t need to think about it, it simply happens).
The main problem is that most causes of facial palsy are due to proximal injury of the facial nerve in the area where it exits from the brain stem out through the stylomastoid foramen, the opening in the skull where the nerve exits and starts to spread in the face to innervate the facial muscles. This prevents us in most cases from using the facial nerve on the injured side, and we then need to use another nerve to innervate the facial muscles. This technique provides good voluntary function and often synchroneity.
A Valuable Resource for Those Affected by Facial Paralysis
If you, a loved one, or a patient is affected by facial paralysis, it’s crucial to have accurate, up-to-date information about symptoms and solutions. Board-certified plastic surgeon Dr. Shai Rozen, a specialist in facial paralysis and facial aesthetics, created Your Guide to Facial Paralysis & Bell’s Palsy to be a readily accessible resource for all.
This downloadable, printable e-book makes it easy to understand:
- How paralysis affects the face
- When it’s time to see a specialist
- Common causes of facial paralysis
- The difference between facial paralysis and Bell’s palsy
- Myths and facts
- The latest treatment options
- Answers to common questions
Get your free copy today—to download or view in your web browser—by completing the following fields:

Will I get a completely normal and spontaneous smile when a non-facial nerve is used to reanimate my face?
Initially, patients will need to bite down a bit in order to activate the smile and sometimes eye closure if the nerve to masseter is used. After a few months to a year (this simply varies among patients), patients do not need to bite down in order to smile; they can voluntarily smile without biting down. The main challenge at this point is whether a patient can smile spontaneously.
Ideally, all patients would smile spontaneously, but this outcome varies among individuals. Some of Dr. Rozen’s patients have developed spontaneity after a couple of years, some after 4 to 5 years, and some won’t develop spontaneity but will use their smile voluntarily and effectively.
Can anything be done to increase the chances of spontaneity?
Dr. Rozen performs several procedures that may increase the chances for spontaneity, but strictly speaking, this has yet to be proven. In most cases, several cross facial nerve grafts are added from the healthy side, or nerve grafts are used to bridge the gap from remnant functioning nerves from the injured side in order to increase the chances of developing spontaneity, and at times a blink reflex. Dr. Rozen is happy to discuss these techniques in detail during a consultation.
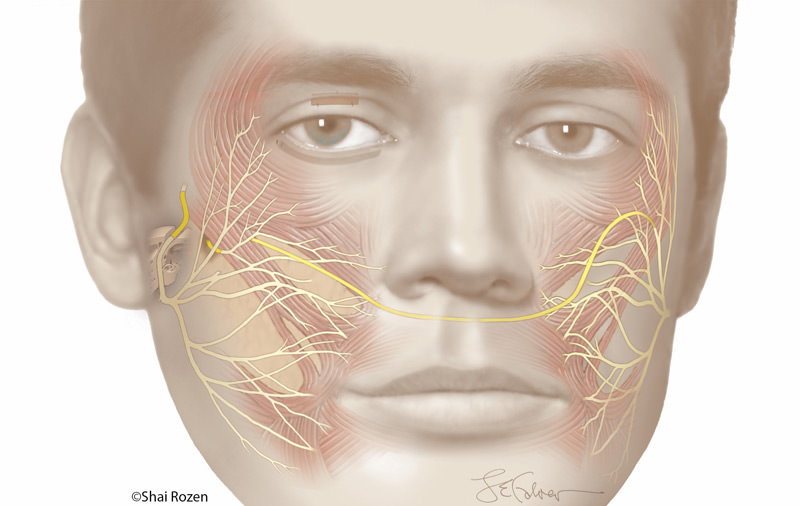
This figure depicts different nerve reconstruction techniques, including nerve transfers, cross facial nerve graft, and intratemporal nerve grafting. Often combining techniques, namely nerve transfers with cross facial nerve grafts, improves tone, synchroneity, and possibly spontaneity over the years and improves function in sub-segments of the face, as published by Dr. Rozen. Orbicularis Oculi Muscle Reinnervation Confers Corneal Protective Advantages over Static Interventions Alone in the Subacute Facial Palsy Patient. Plast Reconstr Surg. 2020 Mar;145(3):791-801. DOI: 10.1097/PRS.0000000000006608. PMID: 32097327. Cover article.
What should I expect after nerve transfer surgery?
Most patients can go home the day of surgery, although Dr. Rozen recommends an overnight stay. Incisions are placed in front of the ears, sometimes extending behind the jaw, so they are minimally noticeable in most patients. If cross facial nerve grafts are performed at the same time, incisions will also be placed in the back of the lower leg through which to harvest the nerves. Pain is not significant after this surgery, but patients are provided with pain medication. Dr. Rozen recommends avoiding anything that raises the blood pressure, strenuous activity, and situations in which you might be hit in the face (holding small children, playing with large dogs, or playing certain sports). Usually, a small drain is inserted and can be removed prior to discharge or in the first clinic visit.
When should I expect to see results from a nerve transfer?
Recovery after facial reanimation is a journey. In most patients, we start seeing motion between 4 to 6 months after the nerve transfers, but this can vary. Variables that may affect the results and recovery time include:
- Duration of paralysis prior to the nerve transfer
- Age of the patient
- Whether the patient has recurrent or spreading disease in some situations such as cancer
Once motion is seen, it is in a way, the beginning of the journey. Patients must practice their smile at home in front of a mirror (please not while driving the car, otherwise Dr. Rozen will have to see you in another setting) and around people in a social setting — initially family, then friends, and then strangers.
This type of practice is recommended for a long time. The patients who constantly practice tend to develop more natural smiles. One of the theories behind this type of practice regimen is that some patients may develop some degree of brain plasticity, which means that certain areas in the brain that are originally dedicated to the action of the donor nerve change function to assist in smiling.
When additional cross facial nerve grafts are used, their effect on the smile may take several years to develop after the surgery. There are quite a few additional factors that dictate how natural a smile is, but this is beyond the scope of this section and can be discussed with Dr. Rozen in person.
Next Steps
If you or a loved one is affected by facial paralysis, Dr. Rozen and his team are ready to help with genuine compassion and the latest treatments available. Request a consultation to meet with Dr. Rozen at UT Southwestern.